Type 2 diabetes mellitus (T2DM) has long been considered a progressive, chronic disease. While medications can help manage blood sugar, durable remission has remained elusive—until recently. A groundbreaking clinical trial led by Dr. Philip Schauer at the Cleveland Clinic has provided compelling evidence that bariatric surgery for type 2 diabetes can do more than help patients lose weight—it can actually reverse the disease.
Why Bariatric Surgery for Type 2 Diabetes Mattered
The STAMPEDE trial (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) asked a bold question: can surgery be more effective than intensive medical therapy in treating T2DM? Importantly, it also included patients who weren’t severely obese—those with a BMI as low as 27 kg/m²—a group traditionally excluded from surgical consideration.
STAMPEDE Trial Design on Bariatric Surgery for Type 2 Diabetes
The trial enrolled 150 patients with poorly controlled type 2 diabetes. All participants received intensive medical therapy, including lifestyle counseling, medications, and insulin if needed. But two groups also underwent bariatric surgery:
- Roux-en-Y gastric bypass
- Sleeve gastrectomy
Researchers followed these patients for over five years, tracking blood sugar levels, weight, medication use, and overall health.
Key Findings from Bariatric Surgery for Type 2 Diabetes
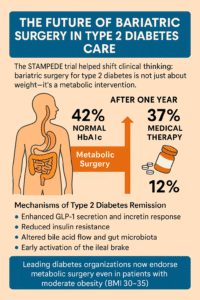
At one year, patients who had surgery were far more likely to reach normal HbA1c levels (≤6.0%):
- 42% of gastric bypass patients
- 37% of sleeve gastrectomy patients
- Compared to just 12% in the medical therapy group
Even more striking, many patients who underwent surgery were able to stop taking diabetes medications entirely, including insulin.
At the five-year mark, surgery continued to show superior outcomes:
- 29% of sleeve patients and 23% of bypass patients had sustained diabetes remission.
- Only 5% of medically treated patients achieved the same result.
More Than Just Weight Loss
The improvements seen in bariatric surgery for type 2 diabetes weren’t solely due to dropping pounds. While weight loss certainly contributed (patients lost 20–25% of their body weight), other mechanisms played a key role:
- Enhanced GLP-1 secretion and incretin response
- Reduced insulin resistance
- Altered bile acid flow and gut microbiota
- Early activation of the ileal brake, promoting satiety and hormonal rebalancing
These changes support the concept that the gut acts as a metabolic organ, and that redirecting nutrients through surgery reshapes its hormonal landscape in ways that benefit glucose control.
The Future of Bariatric Surgery in Type 2 Diabetes Care
The STAMPEDE trial helped shift clinical thinking: bariatric surgery for type 2 diabetes is not just about weight—it’s a metabolic intervention. Based on these results, leading diabetes organizations, including the ADA and EASD, now endorse metabolic surgery even in patients with moderate obesity (BMI 30–35).
For those battling type 2 diabetes despite optimal medical therapy, surgery is no longer a last resort—it’s a transformative, evidence-based solution